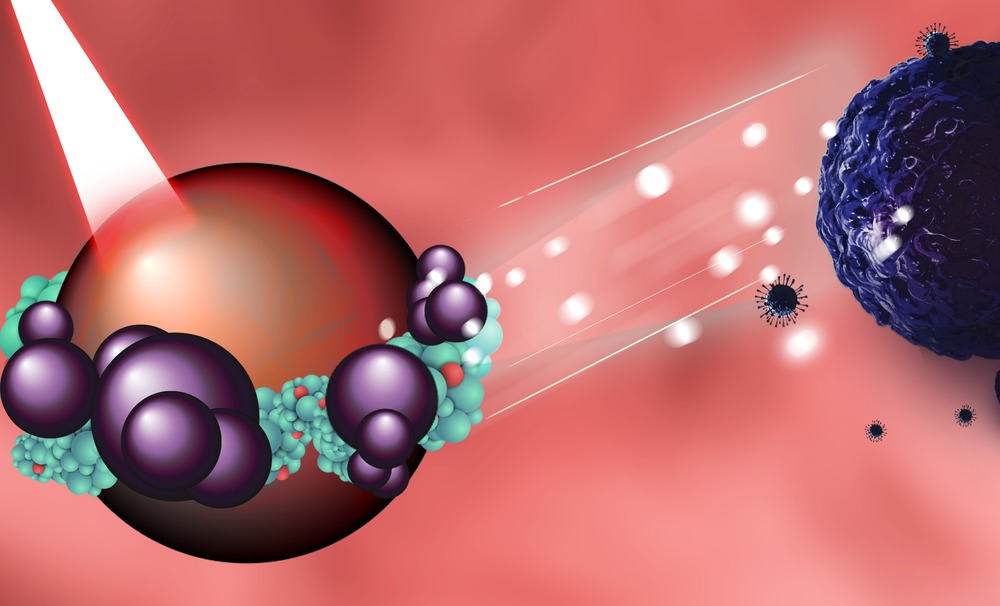
A team of materials scientists from NUST MISIS together with a team of chemists from MIREA-Russian Technological University have managed to combine a photosensitizer molecule (a converter capable of transmitting the energy of light quanta, available in living tissues, into oxygen and turning it into an active form and highly active radicals, which have a cytotoxic effect) with a magnetic nanoparticle to create an innovative therapeutic system to combat cancer. The nanoparticle is a controlled “locomotive” which researchers have learned to deliver locally to a tumor and track by MRI, and as a therapeutic component, the photosensitive molecule serves as an effective liquidator of pathology. The study results have already been tested in-vivo and published in the international scientific journal Journal of Colloid and Interface Science.
“The photodynamic therapy is a cancer treatment method that uses a combination of special preparations—photosensitizers and light with waves of a certain length. The photosensitizers tend to accumulate in the tumor and when exposed to light with certain wavelengths they produce a special form of oxygen that destroys cancer cells. In addition to destroying cancer cells, photodynamic therapy destroys cancer in two other ways. First, photosensitizers can damage the blood vessels in the tumor, thus disrupting the flow of nutrients to it, and second, they can activate the immune system causing it to attack the cancer cells”, said Mikhail Grin, the project co-author, a Doctor of Chemical Sciences, and head of the Department of Chemistry and Technology of Biologically Active Compounds at MIREA-Russian Technological University.
However, this promising method has a natural limitation, as using a light source also directly affects the internal organ, leading to an uncontrollable accumulation of photosensitizers in the tissue. First, a photosensitizer is introduced into the patient`s body (intravenously or in a cavity). The drug is absorbed by cells throughout the body; at the same time, the photosensitizer accumulates in cancer cells in larger amounts than in healthy cells and also remains in them longer.
Then, doctors irradiate the tumor “saturated” by the “light killers”, a.k.a. the photosensitizers, with the help of optic fibers. Usually, laser installations are the light source for photodynamic therapy. The laser light using fiber optic cables should be immediately aimed at the tumor inside the body. The optical cable can be inserted through an endoscope into the stomach or any other natural openings.
The drug, together with a photosensitizer, spreads throughout the body after being introduced into the body, but doctors can`t know for sure when its concentration will reach the desired maximum in a particular area or organ to immediate begin surgery. Logistically speaking, a patient can`t be kept under the lamps and the surgeon`s scalpel for several hours while simply waiting for the optimal momentum of light irradiation. That is why photodynamic therapy is mainly used only for treating skin cancer. The NUST MISIS research team has solved this problem with an innovative drug that includes bacteriochlorin molecules and magnetic nanoparticles.
“We have managed to successfully combine the photosensitizer-bacteriochlorin and magnetite nanoparticles, which are both a drug deliverer and a contrast agent. We have obtained a new tool that allows us, using MRI,, to effectively monitor the degree of accumulation of molecules in the affected organ, which provides the desired concentration and the shortest possible time of surgery. In general,, this approach is promising for fine-tuning therapeutic complexes and significantly scales the method of photodynamic therapy”, said Maxim Abakumov, the project co-author and Head of NUST MISIS`s Biomedical Nanomaterials Laboratory.
The research team has already tested the new method in-vivo and has obtained good intermediate results — the “light killers” immobilized on magnetic nanoparticles were successfully delivered to cancer cells and caused the photo-induced death of cancer cells in lab mice.